Cholesterol Intake Effects Insulin Production
What are the roles of lipoproteins and cholesterol in the body? Consider the interplay of insulin and cholesterol. How does a client’s insulin level impact his/her level of cholesterol? What is the current standard of care for someone who presents with elevated cholesterol? In what ways does this current standard of care affect insulin levels? Outline a nutritional protocol to help your client address his/her concerns of high cholesterol. Include labs might you request from your client’s primary care provider to assist you in designing this protocol. (600 words)
Lipids are hydrophobic: they are non-polar and insoluble in water. This means that they cannot dissolve in blood and rely on special particles for transport. These particles are called lipoproteins. Lipoproteins are a group of proteins synthesized in the small intestine and liver that transport hydrophobic lipids throughout the body. Lipoproteins are made up of lipids and proteins. The hydrophobic lipid portion of lipoproteins is placed in the core, while the hydrophilic protein portion is placed in the periphery of the particle. This particular structure is what allows lipoproteins to travel in the blood and transport lipids through the body.
Find Out What The Different Types of Lipoproteins and Their Names
There are different types of lipoproteins, and they are named according to the density of their content: chylomicron, chylomicron remnant, very low density lipoprotein (VLDL), intermediate density lipoprotein (IDL), low density lipoprotein (LDL), and high density lipoprotein (HDL). Chylomicrons are the least dense while HDL are the densest.

The lipids present in lipoproteins are triglycerides, phospholipids, free cholesterol, and cholesterol ester. Cholesterol is a high-molecular-weight alcohol, and it comes from two sources: exogenous (dietary cholesterol contained only in food from animals) and endogenous (manufactured by the liver). Cholesterol has several vital functions within the body. It gives our cells stability and stiffness. It is a precursor for the synthesis of steroid hormones, vitamin D, and bile, and it acts as an antioxidant. Cholesterol is needed for serotonin function, and low levels of cholesterol have been linked to aggressive behavior, violence, depression, and suicidal tendencies. Breast milk is rich in cholesterol, and infants and children need cholesterol-rich foods for proper development of the brain and nervous system. Cholesterol is also considered the “duct tape” of the body, used to repair damaged tissues.
Cholesterol and Heat Exposure
Cholesterol can become damaged upon exposure to heat and oxygen. Oxidized cholesterol is found in foods like fast foods, fried foods, margarines, baked goods, and foods that are deep fried in rancid vegetable oils.
Several studies reveal that prolonged exposure to insulin is linked to higher levels of lipid peroxidation markers in LDL. For this reason, we need to be aware that clients suffering from hyperinsulinemia will present higher levels of LDL compared to clients with normal blood sugar metabolism. The cholesterol guidelines from the American College of Cardiology and American Heart Association are as follows: patients with arterial plaques and otherwise healthy patients with LDL-C levels greater than or equal to 190 mg/dl are advised to drastically reduced intake of dietary cholesterol and are prescribed high-intensity statin therapy (or maximum tolerated statin therapy). Diabetic patients between the ages of 40 and 75 with LDL-C levels greater than or equal to 70 mg/ dl are prescribed moderate-intensity statin. It is disheartening to see such guidelines in place and to read that many expert physicians consider them not aggressive enough. Statins are dangerous medications linked to a host of side effects including memory loss and confusion, liver damage, muscle pain and damage. Statins also activate an immune response that prevents insulin from working correctly, causing an increase in blood sugar and, therefore, a higher incidence of diabetes. While as a nutritionist I cannot recommend against doctor’s orders, it is my duty to provide my clients with the latest research and information necessary to make informed decisions.
What Is High Cholesterol and How To Bring The Levels Down
When working with clients who are concerned about high cholesterol levels, some of the tests that I find helpful are the advanced lipid tests LDL particle number (LDL-P) and apolipoprotein B (apoB) as well as serum insulin test and c-reactive protein. These tests all measure biomarkers that can accurately predict risk of cardiovascular disease.
The nutritional protocol for such clients focuses on an anti-inflammatory diet that supplies high quality proteins, fats, and carbohydrates from low-glycemic vegetables and fruits. The diet removes added sugars, processed foods, fried foods, and vegetable oils. I also help them with stress management techniques and sleep hygiene. Supplements are an important part of nutritional therapy and, while there is no typical protocol, nutrients that are helpful in cases presenting high cholesterol are: chromium: 200-400 mcg with each meal; vitamin E: 200-600 IU d-alpha and d-gamma tocopherol; l-arginine: 700 mg two to three times a day with meals; magnesium orotate: starting with 400 mg and dosed to bowel tolerance; and curcumin: 15-60 mg three times a day. A formulation that I have used with success is Lipid-Sirt from Biotics Research.
References:
Naviglio D. Bad Cholesterol or “Bad” Science? Med chem [Internet]. 2016 [cited 2020 Oct 15];6(1). Available from: https://www.omicsonline.org/open-access/bad-cholesterol-or-bad-science-2161-0444-1000321.php?aid=66755
Shane Ellison — Life Saving Cholesterol Facts [Internet]. [cited 2020 Oct 15]. Available from: https://newswithviews.com/Ellison/shane13.htm
Kendrick M. The great cholesterol con: the truth about what really causes heart disease and how to avoid it. London: John Blake; 2008. 270 p.
Ross AC, editor. Modern nutrition in health and disease. 11th ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2014. 1616 p.
Shils ME, Shike M, editors. Modern nutrition in health and disease. 10th ed. Philadelphia: Lippincott Williams & Wilkins; 2006. 2069 p.
Smith LL. Another cholesterol hypothesis: cholesterol as antioxidant. Free Radic Biol Med. 1991;11(1):47–61.
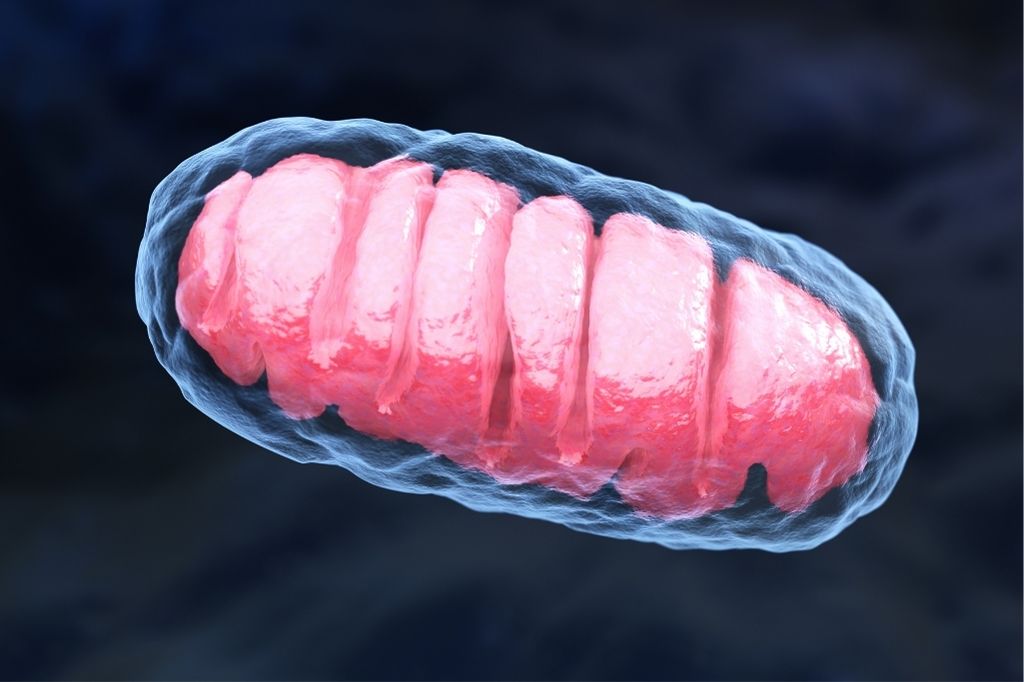
Mei S, Gu H, Yang X, Guo H, Liu Z, Cao W. Prolonged Exposure to Insulin Induces Mitochondrion-Derived Oxidative Stress through Increasing Mitochondrial Cholesterol Content in Hepatocytes. Endocrinology. 2012 May 1;153(5):2120–9.
Colas R, Pruneta-Deloche V, Guichardant M, Luquain-Costaz C, Cugnet-Anceau C, Moret M, et al. Increased lipid peroxidation in LDL from type-2 diabetic patients. Lipids. 2010 Aug;45(8):723–31.
Grundy Scott M., Stone Neil J., Bailey Alison L., Beam Craig, Birtcher Kim K., Blumenthal Roger S., et al. 2018
Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation [Internet]. 2019 Jun 18 [cited 2020 Oct 16];139(25). Available from: https://www.ahajournals.org/doi/10.1161/CIR.0000000000000625
Master SR, Rader DJ. Beyond LDL Cholesterol in Assessing Cardiovascular Risk: apo B or LDL-P? Clin Chem. 2013 May 1;59(5):723–5

Francesca Interviewed on Podcast Business News
Steve Harper Interviews Francesca Orlando Owner of Healthful Living San Diego
Listen here –>> https://podbay.fm/p/podcast-business-news-network-platinum/e/1663078902

Food Consumption And Body Metabolism
Our total daily energy expenditure (TDEE) is dictated by three factors: resting metabolic rate (RMR), which is the number of calories our body needs to perform metabolic functions when it is at rest; the number of calories burnt through physical activity, non-exercise activity thermogenesis (NEAT), and exercise; and the number of calories needed to digest and absorb food. This is called diet-induced thermogenesis (DIT) or thermal effect of feeding (TEF).
Total daily energy expenditure varies from individual to individual and across age, sex, total body weight, physical activity, percentage of fat free mass (FFM), also called lean body mass, versus fat mass (FM), as well as hormones; all play a role in TDEE. In general, RMR accounts for 60% of TDEE, physical activity account for 25-35% of TDEE, and DIT accounts for 5-15% of total energy expenditure.
How Is Food Converted Into Usable Energy?
The foods and beverages that we consume are combined with oxygen and converted into energy in the form of ATP. They also provide the building blocks used to make hormones and enzymes to grow and repair tissue as well as many other processes. When we eat, digest and assimilate food we burn calories. Diet-induced thermogenesis begins immediately after we eat and can last several hours, depending on the macronutrient composition of the meal. The word thermogenesis comes from the Greek θερμός (thermos) and γένεση (genesis), and it means the creation of heat. Not only does DIT create heat during food digestion and absorption, but it also (by a mechanism still not completely understood) activates the sympathetic nervous system which causes the body to produce heat in brown adipose tissue (BAT). BAT is only stimulated by cold temperatures (shivering) and food consumption.
What Exactly Is A Calorie?
A calorie is a unit of energy. It would be simple to think that a calorie is a calorie and that, therefore, 100 calories of steak are the same as 100 calories of brownies, or butter, or broccoli. But different macronutrients require different amounts of ATP to be metabolized and stored. This is why different macronutrients have different thermogenic effects, and DIT can vary greatly depending on the macronutrient composition of our diet.
Protein and alcohol have the highest thermic effects. The DIT for protein is calculated to be between 20 to 30%; the DIT of alcohol is between 10 and 30%. The thermic effect of carbohydrates is between 5 and 10%, and fat has the lowest reported DIT: 0 to 3%. This means that given the same number of calories, meals rich in protein, fat, carbohydrate, or alcohol have different effect on energy expenditure.
Studies show that postprandial thermogenesis in healthy subjects is increased 100% on a high-protein/low-fat diet versus a high-carbohydrate/low-fat carbohydrate diet. In addition, compared to fats and carbohydrates, protein consumption also provides increased satiety. Satiety scores were higher during high protein/high carbohydrate meals versus high fat meals. For these reasons, high protein diets are favored for weight loss as well as for weight maintenance.
How Does Food Effect Metabolism?
When researching the effects of food on metabolism, the next logical question to address is the following: would eating many smaller meals burn more calories than eating one to two larger meals in a 24-hour period? I found contradicting studies when reviewing the literature. Some studies showed that nibbling throughout the day caused a greater caloric expenditure, while other studies showed that consuming larger meals was linked to greater caloric expenditure. It seems that when it comes to meal frequency and metabolism the jury is still out.
There are other nutrients that stimulate metabolism and cause thermogenesis without contributing any calories. These nutrients are caffeine, capsaicin, and cold water. Caffeine is an alkaloid found in coffee beans, tea leaves, and cocoa beans. It is a stimulant and studies show that a cup of coffee can boost metabolism by 3-11%. A study also showed that caffeine may affect lean people more than overweight people as fat burning in lean women increased by 29% with caffeine consumption but obese women registered an increase of only 10%. Capsaicin is a compound found in chili peppers that stimulates metabolism and helps reduce energy intake. Finally, consuming water increases metabolism by 10-30% for about an hour. Cold water may promote an even greater caloric expenditure, as the body uses extra energy to raise the water temperature to body temperature.
References:
Raben A, Agerholm-Larsen L, Flint A, Holst JJ, Astrup A. Meals with similar energy densities but rich in protein, fat, carbohydrate, or alcohol have different effects on energy expenditure and substrate metabolism but not on appetite and energy intake. Am J Clin Nutr. 2003 Jan;77(1):91–100.
Westerterp-Plantenga MS, Rolland V, Wilson SA, Westerterp KR. Satiety related to 24 h diet-induced thermogenesis during high protein/carbohydrate vs high fat diets measured in a respiration chamber. Eur J Clin Nutr. 1999 Jun;53(6):495–502.
Acheson KJ: Influence of autonomic nervous system on nutrient-induced thermogenesis in humans. Nutrition. 1993, 9 (4): 373-80.
Hermsdorff HHM, Volp ACP, Bressan J. [Macronutrient profile affects diet-induced thermogenesis and energy intake]. Arch Latinoam Nutr. 2007 Mar;57(1):33–42.
Jequier E. Thermogenic responses induced by nutrients in man: their importance in energy balance regulation. Experientia Suppl. 1983;44:26–44.
Scott CB, Devore R. Diet-induced thermogenesis: variations among three isocaloric meal-replacement shakes. Nutrition. 2005 Jul 1;21(7):874–7.

The B Vitamins and Their Multilayered Importance In Human Physiology
Folate, Vitamin B12, Vitamin B6, Choline
B vitamins are a class of water-soluble vitamins that are essential to maintain health and to carry out a host of metabolic functions. There are 8 different B vitamins that are necessary for several organs and systems to function optimally. B vitamins are utilized for cellular functioning, carbohydrate metabolism and the production of red blood cells. They are also needed for healthy skin and neurotransmitter formation. Symptoms of B vitamin deficiency vary from fatigue to anemia, nervous system dysfunction, compromised immunity and skin issues. While over consumption of B vitamins from food sources is quite rare and generally not worrisome, dangerously high intake of B vitamin through supplementation leads to hypervitaminosis B. This condition comes with side effects that include liver problems, blurry vision, high blood sugar, and numbness.
What Is Folate?
Folate is needed to produce healthy red blood cells; it reduces the risk of neural tube defects such as spina bifida and, together with vitamin B12 and vitamin C, is an important coenzyme in the synthesis of nucleic acids and the metabolism of amino acids. Optimal folate intake helps in the prevention of folate deficiency anemia.
The Importance of B12
Vitamin B12 is an important factor for the formation of red blood cells, and it is essential in preventing megaloblastic anemia. Vitamin B12 is important for DNA synthesis. Cellular metabolism is dependent on this vitamin, which has a role in the metabolism of fatty acids as well as amino acid synthesis. Vitamin B12 is also necessary for the absorption of folate, and it is necessary for conversion of carbohydrates into glucose. Vitamin B12 also plays a role in white blood cell formation, affecting immune system function.
What To Know About Vitamin B 6
Vitamin B6 (Pyridoxine) exists in various coenzyme forms (pyridoxal 5 phosphate (PLP) and Pyridoxamine 5 phosphate (PMP)). It plays a role in over 100 enzyme reactions, and it is involved in the metabolism of protein, carbohydrates, and lipids. Vitamin B6 is essential for brain development and for immune function. It is vital to synthesize neurotransmitters and to ensure adequate levels of homocysteine. It is also essential for gluconeogenesis, glycogenolysis, and hemoglobin formation. Vitamin B6 works synergistically with folate and vitamin B12 to reduce homocysteine levels. High level of homocysteine is a risk factor in heart disease. While the mechanisms aren’t fully understood, it appears that high homocysteine levels can damage arteries, leading to atherosclerosis and blood clots.
What You Need To Know About Choline
Choline is an organic, water-soluble compound similar to B vitamins. It is manufactured in the liver, and it is also found in foods such as liver, muscle meat, fish, eggs, beans, wheat germs, and nuts. Choline is essential in metabolism, and it is needed for cell membrane integrity. It is important for DNA synthesis, cell signaling, fat transport and metabolism. Choline is necessary to make acetylcholine, an important neurotransmitter; therefore, it is crucial for the nervous system. Choline is a source of methyl groups and is needed to produce two major phospholipids (phosphatidylcholine and sphingomyelin) crucial to cell membranes.

What is the RDA level for each of the vitamins? What is the upper limit for each of the vitamins and What are the signs or symptoms of deficiency and toxicity for each of the vitamins?
The RDA for vitamin B6 varies depending on age, sex, and for women RDA changes also during pregnancy and breastfeeding. RDA for babies from birth to six months is 0.1mg; it is 0.3mg for babies from 7 months to 1 year of age. From 1 to 3 years it is 0.5 mg, 4 to 8 years is 0.6 mg while 4 to 8 years 0.6 mg, 9-13 years is 1.0 mg. RDA for males and females between 19 to 50 years is 1.3 mg. RDA of vitamin B6 for males above 51 years is 1.7 mg and for females it is 1.4 mg.
The RDA for vitamin B12 is dependent on age. The RDA for breastfeeding mothers is 2.8 mcg, while for pregnant teens and women it is 2.6 mcg. Teens and adults are recommended to take 2.4 mg per day of vitamin B12. The RDA for children is 1.2 mcg for the age group 4-8 years, and 1.8 mcg for 9 to 13 years. Infants up to 6 months need 0.4 mcg of vitamin B12 per day; the recommendation for infants 7 to 12 months is 0.5 micrograms per day, and children between 1-3 years require 0.9 mcg per day.
The RDA for folate is also dependent on age. Women and men above 19 years should take 400 mcg of dietary folate equivalents (DFE) per day. The RDA for pregnant women is 600 mcg per day, while RDA for lactating women is 500 mcg. The RDA for people who habitually consume alcohol is at 600 mcg.
The Office of Dietary Supplements states that there is insufficient data to establish the RDA for choline; however, adequate intakes (AI) are available. AI is defined as the “recommended average daily nutrient intake level based on approximations of observed mean nutrient intake by a group (or groups) of apparently healthy people that are assumed to be adequate” (Dietary Reference Intakes: applications in dietary assessment). The AI for individuals above 19 years is 550 mg/day for males and 425 mg/day for females. The AI for pregnant women is 450 mg/day, and for lactating women it is 550mg/day. AI is used as a reference levels when there is not enough evidence to develop an RDA.
Choline deficiency can damage the muscles, liver, and it is linked to the development of nonalcoholic fatty liver disease (NAFLD). Most people in the US consume less than the daily requirement of choline; however, thanks to endogenous production of choline by the liver, deficiency in healthy and non pregnant individuals is rare. High doses of choline can cause dizziness and can lower blood pressure. Choline toxicity can also cause also vomiting, increased sweating, salivation, and it can cause fishy body odor.

Vitamin B 12 deficiency causes fatigue, weakness, constipation, loss of appetite, weight loss, and megaloblastic anemia. It also leads to numbness, balance problems, depression, dementia, and confusion. Vitamin B12 toxicity is rare, and it generally manifests with diarrhea, itching, blood clots, numbness of the extremities, and allergic reactions.
Excessive folate intake masks the symptoms of vitamin B 12 deficiency and can cause damage to the nervous system. Its deficiency mainly leads to folate deficiency anemia, diarrhea, gray hair, peptic ulcer, poor growth, glossitis, and ulcers in the mouth.
It is rare to have an isolated deficiency of vitamin B6. While uncommon, vitamin B6 deficiency is associated with microcytic anemia, cheilosis, dermatitis, glossitis, depression, confusion, and a weakened immune system. An excess of the vitamin B6 leads to sensory neuropathy, ataxia, skin lesions, photosensitivity, nausea, and heartburn. These signs and symptoms are dose-specific.
Where are these vitamins found in the diet and what may impede availability and absorption? How does the concept of food poverty impact a client’s ability to obtain these vitamins?
Vitamin B6 is found in a variety of foods, including salmon, beef, liver, pork, potatoes, bananas, and avocado. Other sources include fortified cereals, poultry, pistachio nuts, and non-citrus fruits.
Beef liver is a great source of folate, and boiled spinach comes right behind. Other good sources include broccoli, leafy green vegetables, peas, kidney beans, chickpeas, and fortified cereals. Pregnant women should take folate supplements and consume foods high in folate to prevent neural tube defects.
The best sources of vitamin B12 are liver and clams. Other good sources are meat, fish, milk, cheese, eggs, dairy, and fortified cereals.
Dietary sources of choline include meat, poultry, fish, milk, eggs, gravies, salads, nuts and seeds, and wheat germ.
Several factors can hinder the absorption and availability of vitamins. Various medications can affect the absorption of various vitamins like vitamin B6. These medications include anti-seizure drugs, the bronchodilator theophylline, and antibiotics like cycloserine. The mechanisms for drug-nutrient interactions vary as well. For instance, cycloserine increases the urinary loss of pyridoxine. Availability and absorption of vitamin B12 are also affected by various gastrointestinal conditions like ulcers, inflammatory bowel disease and other digestive disorders, surgical conditions like gastrostomy, and, of course, medications. The medications include chloramphenicol, omeprazole, cimetidine, and metformin. It is worth noting B vitamins are also best absorbed from food sources; however, folate supplementation is needed in pregnancy and some studies show that supplemental folate is better absorbed than dietary folate (85% bioavailability of supplemental compared to 50% from food sources). It is important to identify factors that can affect the vitamins’ availability and to develop proper strategies that will ensure that our clients have optimal intake and absorption.
What Happens When Food Poverty Is A Significant Component In Mal-nutrition?
Food poverty is the inability to access or purchase foods that make up a healthy diet. In other words, food poverty reduces access to the healthy foods that provide an abundance of vitamins and minerals. Food poverty is linked to malnutrition, obesity, vitamin deficiencies, weakened immune system and other diseases, and disordered eating (people living in food insecurity tend to eat even when not hungry, as a guard against food uncertainty). Since food poverty translates to limited access to healthy foods, people affected by food poverty do not meet RDAs and AI of vitamins and minerals.
References:
Stipanuk MH, Caudill MA, editors. Biochemical, physiological, and molecular aspects of human nutrition. 4th ed. St. Louis, Mo: Elsevier; 2019. 959 p.
Bjørndal B, Bruheim I, Lysne V, Ramsvik MS, Ueland PM, Nordrehaug JE, et al. Plasma choline, homocysteine and vitamin status in healthy adults supplemented with krill oil: a pilot study. Scandinavian Journal of Clinical and Laboratory Investigation. 2018 Nov 17;78(7–8):527–32.
Kennedy DO. B vitamins and the brain: mechanisms, dose and efficacy—a review. Nutrients. 2016 Feb;8(2):68.
Office of dietary supplements – choline [Internet]. [cited 2020 Nov 15]. Available from: https://ods.od.nih.gov/factsheets/Choline-HealthProfessional/
Office of dietary supplements – vitamin b6 [Internet]. [cited 2020 Nov 15]. Available from: https://ods.od.nih.gov/factsheets/VitaminB6-HealthProfessional/
Office of dietary supplements – vitamin b12 [Internet]. [cited 2020 Nov 15]. Available from: https://ods.od.nih.gov/factsheets/VitaminB12-HealthProfessional/
Vitamins and minerals – B vitamins and folic acid [Internet]. nhs.uk. 2017 [cited 2020 Nov 15]. Available from: https://www.nhs.uk/conditions/vitamins-and-minerals/vitamin-b/
Sobczyńska-Malefora A, Harrington DJ. Laboratory assessment of folate (Vitamin b9) status. Journal of Clinical Pathology. 2018 Nov 1;71(11):949–56.
Siddiqui F, Salam RA, Lassi ZS, Das JK. The intertwined relationship between malnutrition and poverty. Front Public Health [Internet]. 2020 [cited 2020 Nov 15];8. Available from: https://www.frontiersin.org/articles/10.3389/fpubh.2020.00453/full